The UroCuff Test
The UroCuff Test is a non-invasive pressure-flow study for patients reporting lower urinary tract symptoms (LUTS) such as urgency, frequency, nocturia, and incomplete emptying, or who have noted other changes in voiding patterns.
The UroCuff provides the urologist with natural fill pressure-flow data for assessment of voiding disorders.
Key Benefits of The UroCuff:
- Clinically proven to accurately measure voiding pressure.
- Differentiates between bladder outlet obstruction (BOO) and poor bladder contractility.
- Simple to perform.
- More comfortable for the patient than a traditional catheterized urodynamic study.
The UroCuff Test is the new standard in non-invasive LUTS assessment. Moreover, the UroCuff offers your practice a LUTS patient management platform providing better clinical outcomes and greater efficiency. The UroCuff is simply a better way to manage LUTS patients in the today’s healthcare system.

PFS Score® diagnostic testing is available exclusively with UroCuff®-DC.
How It Works
The UroCuff Test simultaneously measures urine flow rate and bladder pressure to assist in determining the underlying cause of the voiding disorder. Bladder pressure is measured non-invasively with a penile cuff instead of a catheter. When the patient is ready to void, a small cuff is fitted to the penis, and the patient is asked to void into the flow meter. When voiding has commenced, the cuff will apply pressure until the urine flow is reduced or stopped. Inflation cycles are repeated until the void is complete. The cuff pressure required to interrupt flow equals bladder pressure at the time of interruption.
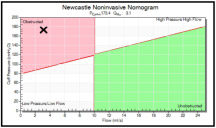
Once the test is complete, the UroCuff report summarizes the pressure-flow data on a modified nomogram. Shown to the right are nomograms from two different patients that had identical maximum flow rates of 3.1 ml/s. These patients are therefore both “low flow rate” patients, and they would present with the same flow rates when the traditional uroflow test is prescribed. However, the UroCuff nomogram on the top reveals that the first patient has a low bladder pressure, while the nomogram on the bottom reveals the second patient has high bladder pressure. Click on either of these nomograms to see the complete UroCuff report.
Optionally, one or two surface EMG electrodes may be applied to the patient to monitor skeletal muscle function during the void:
a. Perineal EMG Placement–to monitor sphincter activity.
b. Abdominal EMG Placement–to monitor abdominal straining.
Equipment
The UroCuff Test has a simple and consistent touch-screen interface that guides the clinician step-by-step through each test. The hardware consists of the following components:
- UroCuff Instrument Console.
- UroFlow™ scale.
- All-in-one Panel PC.
- Commode.
- Printer.
- All necessary software, cabling, & accessories.

Clinical Literature
Peer Review Publications
There is a large body of peer-reviewed clinical literature on the UroCuff Test. Sample citations along with abstracts and links to the complete documents provided below. Please contact SRS Medical for a complete listing of peer-reviewed clinical literature.
UroCuff Non-invasive Pressure Flow Studies in the Evaluation of Men with Lower Urinary Tract Symptoms Secondary to Benign Prostatic Hyperplasia: A Review of 50,000 Patients. Kaplan SA, Kohler TS, Kausik SJ. The Journal of Urology (2020).
Objective
The UroCuff Test is a non-invasive pressure-flow study (PFS) used to manage men with lower urinary tract symptoms (LUTS). UroCuff Tests were performed on men with LUTS to evaluate voiding characteristics and quantify changes in urodynamic parameters with age.
Materials and Methods
This cross-sectional study included all UroCuff Tests performed at 103 urology practices in the US. Tests were de-identified prior to collection and analysis. Inclusion criteria required: initial PFS with subsequent tests excluded, voided volume (VV) ≥ 50 ml, at least one cuff inflation, and patient age > 20 years. Pressure (Pcuff), maximum flow rate (Qmax), flow rate efficiency (FRE; Qmax/Pcuff), VV and post void residual (PVR) were plotted by age and stratified by Newcastle Noninvasive Nomogram (NNN) category.
Results
50,680 patients, 20 – 100 years of age (median 66.0) met inclusion criteria. Median Pcuff was 144.3 cmH2O, 60.8% of patients were categorized in the Obstructed or High Pressure/High Flow NNN quadrants. Median Qmax was 10.9 ml/s, 55.8% had Qmax > 10 ml/s. Median VV and post void residual (PVR) were 219.0 ml and 75.0 ml respectively. All measures deteriorated with age (p<0.0001). Pcuff reflects the compensated/decompensated bladder function lifecycle; values initially increased and reached peak pressure at age 62, then decreased by approximately 0.96 cmH2O/year until age 90.
Conclusion
This study demonstrates that symptomatic patients enter urological practices at different urodynamic stages of bladder function and outlet obstruction, that Pcuff, Qmax, VV, FRE and PVR deteriorate with age, and UroCuff is a sensitive evaluation of bladder performance.
Comparison of Penile Cuff Test and Conventional Urodynamic Study Prior to Photoselective Vaporization of Prostate for Benign Prostate Hyperplasia Using a 120 W GreenLight High Performance System Laser. Kim KS, Choi YS, Bae WJ, el al. Journal of Clinical Medicine (2020).
Objective
To compare the utility of the penile cuff test (PCT) and the conventional urodynamic study (UDS) for the preoperative assessment of patients undergoing scheduled photoselective vaporization of the prostate (PVP) for benign prostate hyperplasia (BPH).
Materials and Methods
Fifty-nine patients with voiding lower urinary tract symptoms (LUTS) underwent a simultaneous PCT and conventional UDS before PVP. The modified International Continence Society (ICS) nomogram was used to confirm bladder outlet obstruction after measuring maximum urinary flow rate and highest pressure at flow interruption. The PCT and UDS results, in terms of modified ICS nomogram predictions, were compared. Their sensitivities, specificities, and positive and negative predictive values were calculated.
Results
Thirty-six patients were diagnosed as obstructed and 23 as non-obstructed/equivocal using the modified ICS nomogram during the PCT. All 36 of the first group were confirmed as obstructed by UDS. Of the 23 diagnosed as non-obstructed/equivocal by the PCT, 14 were confirmed to be non-obstructed by UDS, with nine diagnosed as obstructed. The PCT showed a sensitivity of 80% and a specificity of 100%. The positive and negative predictive values were 100% and 60.9%, respectively.
Conclusion
The PCT’s high sensitivity and specificity suggest that it may provide diagnostic information about bladder outlet obstruction before PVP for patients with voiding LUTS. Evidently, the PCT has the potential to be used for some patients as a screening alternative to invasive UDS.
Can the Penile Cuff Test Predict the Outcome of Holmium Laser Enucleation of the Prostate for Benign Prostatic Obstruction? Ko KJ, et al. Urology (2019).
Objective
To determine whether the penile cuff test can predict surgical outcomes prior to Holmium laser enucleation of the prostate for benign prostatic obstruction.
Materials and Methods
Men scheduled to undergo Holmium laser enucleation of the prostate were enrolled in this study, and all patients underwent the penile cuff test prior to and 3 months after surgery. Patients were categorized as obstructed, nonobstructed, or uncertain by nomogram. Surgical outcomes were assessed by evaluating changes in their international prostate symptom score, quality of life index, and maximum flow rate preoperatively and 3 months postoperatively. The proportion of patients with good outcomes was compared among nomogram-classified groups, and postoperative changes in position on the nomogram were assessed.
Results
A total of 125 patients were analyzed. After surgery, the overall treatment efficacy and symptomatic treatment efficacy were not different between obstructed and nonobstructed patients. However, the maximum flow rate and quality of life score were significantly higher after surgery in obstructed patients compared to nonobstructed patients. After surgery, 75.7% of patients with obstruction and 63.6% of patients categorized as uncertain for obstruction transitioned to the nonobstructed group, while 77.3% of nonobstructed patients remained in the nonobstructed group.
Conclusion
The penile cuff test can be used in patients with bladder outlet obstruction to predict good functional outcome and improved quality of life following treatment with Holmium laser enucleation. After Holmium laser enucleation of the prostate, the majority of patients were classified as nonobstructed.
Diagnosing bladder outlet obstruction using the penile cuff test in men with lower urinary tract symptoms. Ko, K J, et al. Neurourology and Urodynamics (2017).
Objective
The current standard diagnostic test to evaluate bladder outlet obstruction (BOO) is pressure-flow study (PFS). The penile cuff test (PCT) was introduced as a non-invasive alternative to PFS to determine the isovolumetric bladder pressure and also flow rate. The aim of the study was to evaluate the diagnostic accuracy and acceptability of the PCT, compared to those of PFS, in the assessment of BOO in men.
Materials and Methods
A total of 146 consecutive men with an International Prostate Symptom Score (IPSS) >12 and lower urinary tract symptoms (LUTS) for >6 months were included in this single-institution, prospective, diagnostic study. The primary outcome was to evaluate the diagnostic accuracy of PCT. Secondary outcomes included pain severity measured on a visual analog scale (VAS), procedure time, and adverse events. In addition, the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were estimated.
Results
Based on the PFS results, the sensitivity of PCT was 89.7%, the PPV 54.2%, the specificity 71.8%, and the NPV 94.9%. The mean pain VAS for the PFS and PCT were 5.04 ± 2.17 and 1.83 ± 1.98, respectively (P < 0.0001). The mean procedure time for PCT (6.3 ± 0.6 min) was shorter than that of PFS (23.3 ± 2.2 min) (P < 0.0001). There were no adverse events reported during PCT.
Conclusion
Given its high NPV, PCT may be an efficient screening test for BOO in men. In addition, PCT is advantageous over PFS with regard to its short procedure time and acceptable tolerability.
The UroCuff test: a non-invasive alternative to pressure flow studies in adult males with lower urinary tract symptoms secondary to bladder outlet obstruction. Matulewicz, RS, & Hairston, JC. The Canadian Journal of Urology (2015).
Introduction
To assure that patients with lower urinary tract symptoms (LUTS) benefit from interventions, urologists must practice careful selection of surgical candidates. Currently, 15%-30% of men do not benefit optimally from these invasive and potentially morbid procedures. Success rates following transurethral resection of the prostate (TURP) are higher if bladder outlet obstruction (BOO) is confirmed prior to the procedure by invasive pressure flow studies (PFS). However, PFS may not be performed because of many reasons. We report a study of a non-invasive method of assessing BOO.
Materials and Methods
The UroCuff test was compared to invasive urodynamic studies in adult males with lower urinary tract symptoms. Patients undergoing PFS for LUTS presumed to be due to BOO were recruited from a single site to perform a penile cuff test (UroCuff) at the same time as PFS. Standard PFS were performed followed immediately by a penile cuff test in the same test setting. The results were compared using basic statistical analysis.
Results
A total of 19 men were evaluated by both PFS and UroCuff evaluation. Using PFS as the gold standard, the positive predictive value of the UroCuff penile cuff test to diagnose BOO was found to be 92%. The sensitivity of the UroCuff test for detecting BOO was 75%. When compared to PFS, patients preferred the UroCuff 100% of the time.
Conclusion
The UroCuff test is accurate in predicting BOO when compared to conventional invasive pressure flow studies in men with LUTS. It is well tolerated and preferred over invasive pressure flow studies.
Non-invasive urodynamics predicts outcome prior to surgery for prostatic obstruction. Losco G, Keedle L, King Q. BJU International (2013).
Objective
To assess whether the penile cuff non-invasive urodynamic test serves as an effective diagnostic tool for predicting outcomes prior to disobstructive surgery for men presenting with voiding lower urinary tract symptoms. Patients with proven urodynamic obstruction do better after surgery. The current gold standard, invasive pressure-flow studies, imposes cost, resource demand, discomfort and inconvenience to patients.
Patients and Methods
Patients undergoing surgery for prostatic obstruction at Palmerston North Hospital had pre-operative non-invasive urodynamics and completed an International Prostate Symptom Score (IPSS). Catheterised patients were excluded. Two months post-operatively they completed a further IPSS score. An improvement of seven or greater was defined as a clinically successful outcome. Results were compared with the outcome predicted by the nomogram supplied with the urodynamic device.
Results
Data was obtained for 62 patients with mean age 70 years (range 49 to 86 years; SD 9 years). Follow-up was complete for all patients. Thirty-eight patients underwent transurethral resection and 24 holmium laser enucleation of the prostate. Mean IPSS score was 21 (range 5 to 35; SD 6) pre-operatively and 11 (range 1 to 31; SD 9) post-operatively. Thirty-five patients were predicted obstructed and 27 not obstructed. 94% of those predicted obstructed had a successful outcome (p < 0.01). 70% predicted as not obstructed did not have a successful outcome after surgery (p < 0.01).
Conclusion
The penile cuff test is an exciting adjunct in the decision to proceed to surgery for prostatic obstruction. Patients predicted to be obstructed have an excellent likelihood of a good surgical outcome, yet 30% of those shown not to be obstructed will still do well. Whilst numbers in our study are small, outcomes compare favourably with published results on invasive urodynamic methods.
Correlation between penile cuff test and pressure-flow study in patients candidates for trans-urethral resection of prostate. Bianchi D, Di Santo A, Gaziev G, Miano R, Musco S, Vespasiani G and Agrò EF. BMC Urology (2014).
Background
Aim of this study was to make a comparison between penile cuff test (PCT) and standard pressure-flow study (PFS) in the preoperative evaluation of patients candidates for trans-urethral resection of prostate (TURP) for benign prostatic obstruction (BPO).
Methods
We enrolled male patients with lower urinary tract symptoms candidates for TURP. Each of them underwent a PCT and a subsequent PFS. A statistical analysis was performed: sensitivity (SE), specificity (SP), positive predictive value (PPV), negative predictive value (NPV), likelihood ratio and ratio of corrected classified were calculated. Fisher exact test was used to evaluate relationships between PCT and maximal urine flow (Qmax): a p-value < 0.05 was considered statistically significant.
Results
We enrolled 48 consecutive patients. Overall, at PCT 31 patients were diagnosed as obstructed and 17 patients as unobstructed. At the subsequent PFS, 21 out of 31 patients diagnosed as obstructed at PCT were confirmed to be obstructed; one was diagnosed as unobstructed; the remaining 9 patients appeared as equivocal. Concerning the 17 patients unobstructed at PCT, all of them were confirmed not to be obstructed at PFS, with 10 equivocal and 7 unobstructed. The rate of correctly classified patients at PCT was 79% (95%-CI 65%-90%). About detecting obstructed patients, PCT showed a SE of 100% and a SP of 63%. The PPV was 68%, while the NPV was 100%.
Conclusion
The PCT can be an efficient tool in evaluating patients candidates for TURP. In particular, it showed good reliability in ruling out BPO because of its high NPV, with a high rate of correctly classified patients overall. Further studies on a huger number of patients are needed, including post-operative follow-up as well.
NHS Evidence Review: Mediplus CT3000 Cuff Machine for Diagnosis of Bladder Outlet Obstruction.
Evidence Reviewed
NHS Centre for Evidence-based Purchasing Verdict – Significant Potential:
The Mediplus CT3000 system offers greater accuracy in diagnosis of BOO than diagnosis based on flow rate measurement alone. Recent results (3) suggest its prediction of outcome from surgery rivals that offered by invasive urodynamic studies, though this has not been conclusively proven by this limited evidence. The invasive approach also provides additional information, and therefore remains the gold standard for the diagnosis of BOO in men. The existing evidence supports the manufacturer’s claim that the CT3000 system has a useful role as an adjunct to current methods. Diagnoses based on CT3000 and urine flow measurement can be compared. Where there is agreement, surgery is indicated, and where there is disagreement or uncertainty, follow up invasive urodynamics are indicated. This approach may well reduce the number of ineffective surgical prostatectomies while also reducing the number of invasive studies, both of which carry associated costs and risks. Independent validating studies on the Mediplus CT3000 cuff system are recommended, and a multi-centre trial is reported to be underway (3). A detailed economic evaluation is also recommended, considering both the costs and consequences of the diagnostic accuracy of the CT3000 system.
Review of invasive urodynamics and progress towards non-invasive measurements in the assessment of bladder outlet obstruction. Griffiths C J, Pickard R S. Indian Journal of Urology (2009).
Purpose
This article defines the need for objective measurements to help diagnose the cause of lower urinary tract symptoms (LUTS). It describes the conventional techniques available, mainly invasive, and then summarizes the emerging range of non-invasive measurement techniques.
Materials and Methods
This is a narrative review derived from the clinical and scientific knowledge of the authors together with consideration of selected literature. The CT3000 UroCuff test was compared to traditional catheter based urodynamic studies in adult males with lower urinary tract symptoms.
Results
Consideration of measured bladder pressure urinary flow rate during voiding in an invasive pressure flow study is considered the gold standard for categorization of bladder outlet obstruction (BOO). The diagnosis is currently made by plotting the detrusor pressure at maximum flow (PdetQmax) and maximum flow rate (Qmax) on the nomogram approved by the International Continence Society. This plot will categorize the void as obstructed, equivocal or unobstructed. The invasive and relatively complex nature of this investigation has led to a number of inventive techniques to categorize BOO either by measuring bladder pressure non-invasively or by providing a proxy measure such as bladder weight.
Conclusion
Non-invasive methods of diagnosing BOO show great promise and a few have reached the stage of being commercially available. Further studies are however needed to validate the measurement technique and assess their worth in the assessment of men with LUTS.
The penile cuff test: A clinically useful non-invasive urodynamic investigation to diagnose men with lower urinary tract symptoms. Harding, C, Robson, W, Drinnan, M, McIntosh, S, Sajeel, M, Giffiths, C, & Pickard, R. Indian Journal of Urology (2009).
Objectives
To summarize the development of a novel non-invasive test to categorize voiding dysfunction in men complaining of lower urinary tract symptoms (LUTS) – the penile cuff test.
Methods
The test involves the controlled inflation of a penile cuff during micturition to interrupt voiding and hence estimate isovolumetric bladder pressure (pves.isv). The validity, reliability, and clinical usefulness of the test were determined in a number of studies in men with LUTS.
Results
The penile cuff test can be successfully performed in over 90% of men with LUTS. The reading of cuff pressure at flow interruption (pcuff.int) gives a valid and reliable estimate of invasively-measured pves.isv and when combined with the reading for maximum flow rate obtained during the test (Qmax) produces an accurate categorization of bladder outlet obstruction (BOO). Use of this categorization prior to treatment allows improved prediction of outcome from prostatectomy.
Conclusion
The penile cuff test fulfils the criteria as a useful clinical measurement technique applicable to the diagnosis and treatment planning of men with LUTS.
Interobserver Agreement for Noninvasive Bladder Pressure Flow Recording With Penile Cuff. McArdle F, Clarkson B, Robson W, Griffiths C, Drinnan M, Pickard R. The Journal of Urology (2009).
Purpose
We assessed variability in interpreting noninvasive measurements of bladder pressure and urine flow between experienced and novice users of the penile cuff.
Materials & Methods
Urodynamicists at 6 sites were asked to use the penile cuff test as part of clinical assessment in 30 men presenting with lower urinary tract symptoms. After a short training period they measured maximum flow rate and cuff interruption pressure from penile cuff test recordings to enable categorization of bladder outlet obstruction using a nomogram. Similar measurements were then made on the same traces by 2 expert observers from the originating center. Interobserver differences were assessed.
Results
Complete agreement on obstruction categorization was seen in 77% of subjects, which increased to 86% when plots positioned on category boundary lines were allocated to the favored category. The 95% confidence limits of interobserver variability in maximum flow rate and cuff interruption pressure measurements were ± 1.7 ml per second and ± 13 cm H2O, respectively, although a small number of studies yielded discrepancies between observers that were larger than expected. They arose from complex recordings but were equally likely between experts as between expert and novice. Investigation of the causes suggested in some cases how such discrepancies may be avoided in the future.
Conclusion
The excellent level of agreement in measurement and categorization after a short training period suggests that introducing the penile cuff test as part of assessment in men with lower urinary tract symptoms would be straightforward.
Multisite Evaluation of Noninvasive Bladder Pressure Flow Recording Using the Penile Cuff Device: Assessment of Test-Retest Agreement. Clarkson B, Robson W, Griffiths C, McArdle F, Drinnan M, Pickard R. The Journal of Urology (2008).
Purpose
We performed a pragmatic study of the penile cuff test, a noninvasive method of categorizing bladder outlet obstruction, at a number of United Kingdom urology centers remote from the originating site. We report the agreement of the test and the subsequent retest using the cuff test in the short term.
Methods
Men requiring urodynamic investigation for lower urinary tract symptoms were recruited from 6 sites to perform a penile cuff test twice at an interval of approximately 4 weeks. Tests were analyzed by a single interpreter to assess differences in the flow rate, cuff interruption pressure and diagnostic categorization in an individual between the 2 tests due to measurement and physiological error.
Results
A total of 136 men (69%) performed 2 suitable cuff tests at a median of 20 days (IQR 8–31). The mean ± SD difference between the 2 tests in the maximum flow rate was 0.2 ± 3.7 ml per second and in cuff interruption pressure was 4.0 ± 26 cm H2O. Of the men 33% changed diagnostic category on the Newcastle nomogram, while 47% maintained a consistent diagnosis of obstruction or no obstruction.
Conclusion
Diagnostic category repeatability was similar to that of conventional urodynamics, although there was greater variability in pressure measurements. This supports widespread routine use of the penile cuff test.
Categorization of Obstruction Using Noninvasive Pressure Flow Measurements: Sensitivity to Change Following Prostatectomy. Sajeel M, Harding C, Robson W, Drinnan M, Griffiths C, Pickard R. The Journal of Urology (2007).
Purpose
We determined whether categorizing men with lower urinary tract symptoms using a noninvasive pressure flow nomogram is sensitive to change following the removal of obstruction.
Materials and Methods
A prospective cohort of men undergoing transurethral prostate resection was recruited, of whom 143 (69%) underwent noninvasive pressure flow study using the penile cuff technique before and 4 months following surgery. Cuff pressure required to interrupt voiding, estimated isovolumetric bladder pressure and maximum flow rate were recorded during a single void. Values were plotted on a nomogram categorizing cases as obstructed (upper left quadrant), not obstructed (lower right quadrant) or diagnosis uncertain (upper right and lower left quadrants). Changes in maximum flow rate, cuff pressure required to interrupt voiding and nomogram position following transurethral prostate resection were then analyzed.
Results
Transurethral prostate resection resulted in an improved flow rate for all diagnostic groups, which was highest for obstructed cases with a mean ± SD increase of 11 ± 6 ml second (p <0.01). Men categorized with obstruction and those placed in the upper right quadrant showed significant decreases in cuff pressure required to interrupt voiding following transurethral prostate resection with a mean decrease of – 45 ± 35 and – 48 ± 32 cm H2O, respectively (p <0.01). The number of cases classified as not obstructed increased from 28 (19%) preoperatively to 114 (80%) after transurethral prostate resection.
Conclusion
Sensitivity to change following the removal of obstruction further validated the usefulness of noninvasive measurement of bladder pressure by the penile cuff test and the categorization of obstruction by the noninvasive nomogram. Decreased isovolumetric bladder pressure following transurethral prostate resection may reflect a return to normal detrusor contraction strength.
Predicting the Outcome of Prostatectomy Using Noninvasive Bladder Pressure and Urine Flow Measurements. Harding C, Robson W, Drinnan M, Sajeel M, Ramsden P, Griffiths C, Pickard R. European Urology (2007).
Purpose
To determine whether categorisation of bladder outlet obstruction (BOO) using measurements of bladder pressure and urine flow obtained by a novel noninvasive medical device (the penile cuff test) improves prediction of outcome from endoscopic prostatectomy (TURP).
Methods
A consecutive cohort of 208 men undergoing TURP following standard assessment in our institution was recruited, and 179 (86%) completed the protocol. Each subject underwent a penile cuff test prior to surgery; outcome was assessed by change in IPSS at 4 mo. The proportion of men with good outcome (>50% reduction in IPSS) was compared according to categorisation by noninvasive bladder pressure and urine flow measurements.
Results
The cuff test was completed by 93% of men with 2% experiencing an adverse event. Men categorised as having BOO by the test (37% of total) had an 87% chance of a good outcome from TURP (p < 0.01), whilst of those deemed not obstructed (19% of total) 56% experienced good outcome (p < 0.01). For the remaining men not categorised in these two groups, 77% had good outcome, which was identical to the result of the cohort as a whole (77%, p = NS).
Conclusion
Urodynamic categorisation using measurements obtained by the noninvasive penile cuff test improves prediction of outcome for men with LUTS undergoing TURP. This finding together with the ease and acceptability of the test suggest its suitability for office-based clinical use to assist men and their physicians in the selection for surgical treatment for relief of LUTS.